If you have recently undergone an ultrasound examination and the report mentions a “hyperechoic liver,” you may be wondering what it means and if it is a cause for concern. In this article, we will explore the causes, symptoms, and treatment options for a hyperechoic liver. So, let’s dive in and find out more about this condition.
What is a Hyperechoic Liver?
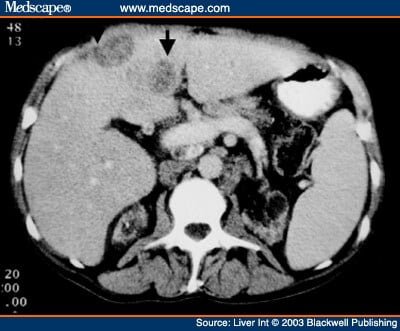
A hyperechoic liver refers to a liver that appears brighter or more echogenic than the surrounding tissues on an ultrasound scan. This increased echogenicity is caused by the reflection of sound waves off the liver tissue, resulting in a brighter appearance on the ultrasound image.
The Causes
There are several possible causes for a hyperechoic liver. Some of the common causes include:
- Fatty liver disease: Accumulation of fat in the liver can cause it to appear hyperechoic on an ultrasound scan.
- Hepatitis: Inflammation of the liver due to viral infections like hepatitis can lead to increased echogenicity.
- Cirrhosis: Advanced liver disease, such as cirrhosis, can cause changes in liver tissue, resulting in a hyperechoic appearance.
- Hemochromatosis: This is a condition characterized by excessive iron deposition in the liver, leading to increased echogenicity.
- Alcohol abuse: Chronic alcohol consumption can cause fatty liver disease and liver inflammation, both of which can contribute to a hyperechoic liver.
Symptoms of Hyperechoic Liver
In most cases, a hyperechoic liver does not cause any specific symptoms. It is often detected incidentally during an ultrasound examination for other reasons. However, if an underlying condition, such as fatty liver disease or cirrhosis, is causing the hyperechoic appearance, you may experience symptoms related to those conditions. Some common symptoms include:
- Fatigue
- Abdominal pain or discomfort
- Jaundice (yellowing of the skin and eyes)
- Swelling in the legs or abdomen
- Unexplained weight loss
Treatment Options
The treatment for a hyperechoic liver depends on the underlying cause. Here are some common treatment options:
- Fatty liver disease: Lifestyle changes, such as maintaining a healthy weight, exercising regularly, and avoiding excessive alcohol consumption, can help improve fatty liver disease.
- Hepatitis: Treatment for hepatitis may involve antiviral medications, rest, and adequate hydration.
- Cirrhosis: Management of cirrhosis focuses on preventing further liver damage, managing complications, and addressing the underlying cause, such as alcohol cessation or treatment for viral hepatitis.
- Hemochromatosis: Treatment for hemochromatosis involves regular blood removal (phlebotomy) to reduce iron levels in the body.
FAQs
Q: Can a hyperechoic liver be reversed?
A: The reversibility of a hyperechoic liver depends on the underlying cause. In some cases, such as fatty liver disease, lifestyle changes can help improve the condition. However, in advanced liver diseases like cirrhosis, the damage may be irreversible.
Q: Is it a sign of cancer?
A: A hyperechoic liver is not typically a sign of cancer. However, certain liver tumors, such as hepatocellular carcinoma, can appear hyperechoic on ultrasound scans. If cancer is suspected, further diagnostic tests may be necessary to confirm the diagnosis.
Q: Can it cause pain?
A: In most cases, a hyperechoic liver does not cause pain. However, if an underlying condition, such as cirrhosis or liver inflammation, is present, you may experience abdominal pain or discomfort.
Conclusion
In conclusion, a hyperechoic liver refers to a liver that appears brighter or more echogenic than the surrounding tissues on an ultrasound scan. It can be caused by various conditions, including fatty liver disease, hepatitis, cirrhosis, hemochromatosis, and alcohol abuse. While a hyperechoic liver itself may not cause specific symptoms, it can be an indicator of an underlying liver condition. Treatment options depend on the underlying cause, and lifestyle changes, medications, and management of complications are often part of the treatment plan. Remember, if you have any concerns about your liver health, it is always best to consult with a healthcare professional for an accurate diagnosis and appropriate treatment.
Fun Fact: Did you know that the liver is the largest internal organ in the human body? It performs over 500 vital functions, including detoxification, metabolism, and production of essential proteins.
Originally posted 2023-03-20 15:28:37.