Singer George Michael died of natural causes related to heart disease and fatty liver, according to the British coroner report released Tuesday. While most people understand the causes of cardiovascular disease, few know anything about fatty liver and how it can lead to adverse health outcomes or — in its most severe stage — death.
The reports surrounding Michael’s death don’t directly suggest that his health ultimately deteriorated due to excess drugs, and alcohol. However, it’s important to recognize these toxins can be destructive to the liver, the body’s main detoxifying organ.
If you have a fatty liver, do not wait and act fast. Sign up to our FREE course
What is a fatty liver?
As alcohol floods the system, the liver starts to form abnormal deposits of fat. This causes inflammation and scarring; eventually the healthy liver tissue is replaced with scar tissue. That’s when your liver stops working and you find yourself on a transplant list.
But alcohol isn’t the only factor — there are more common habits that may lead to the same disease.
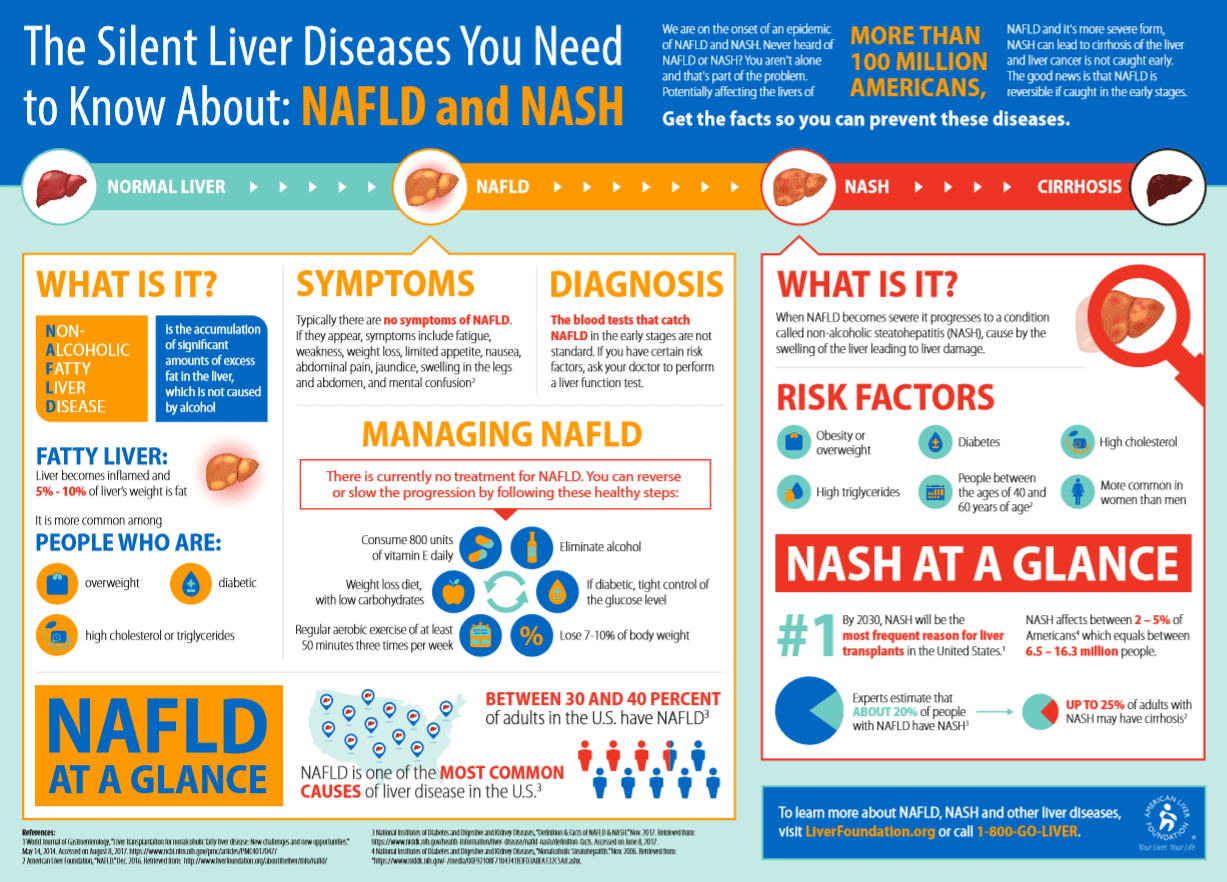
Another type of liver disease is emerging, called Non-Alcoholic Fatty Liver Disease, or NAFLD. It’s caused by being overweight or obese and consumption of too much sugar and processed carbohydrates, along with a sedentary lifestyle and components associated with metabolic syndrome. It’s quickly becoming the number one disease on the liver transplant list.
This fatty liver disease affects 33 percent of the U.S. population, including 6 million children. In fact, it’s the number one liver condition in children.
NAFLD is an independent risk factor for cardiovascular disease, and recent evidence shows that many patients with it are more likely to end up dying from the heart failure before they do liver disease.
What is Fatty Liver Disease?
Fatty liver disease means you have extra fat in your liver. You might hear your doctor call it hepatic steatosis.
Heavy drinking makes you more likely to get it. Over time, too much alcohol leads to a buildup of fat inside your liver cells. This makes it harder for your liver to work.
But you can get fatty liver disease even if you don’t drink a lot of alcohol.
Nonalcoholic Fatty Liver Disease (NAFLD)
Like the name says, alcohol isn’t involved in this condition. Instead, it results largely from metabolic syndrome, an umbrella term for a condition marked by high blood pressure, high levels of bad cholesterol, insulin resistance, and large amounts of belly fat.
There are different types of NAFLD.
Simple fatty liver: This means you have fat in your liver, but you may not have any inflammation in your liver or damage to your liver cells. It usually doesn’t get worse or cause problems with your liver. Most people with NAFLD have simple fatty liver.
Nonalcoholic steatohepatitis (NASH): This is much more serious than a simple fatty liver. NASH means you have inflammation in your liver. You may also have damage to your liver cells. The inflammation and liver cell damage that happen with NASH can cause serious problems such as:
- Fibrosis: scarring of the liver
- Cirrhosis: severe scarring in the liver, which can lead to liver failure and death
- Liver cancer
About 20% of people with NAFLD have NASH.
Alcohol-Related Fatty Liver Disease (ALD)
You might hear this called “ALD.”
Some people don’t have any symptoms. But if your liver becomes enlarged, you may have pain or discomfort on the upper right side of your belly.
ALD is preventable. It usually gets better when you stop drinking alcohol.
If you keep drinking, ALD can cause serious problems. These include:
Alcoholic hepatitis. This is swelling in the liver that can cause fever, nausea, vomiting, belly pain, and jaundice (yellowish skin and eyes).
Alcoholic cirrhosis. This is a buildup of scar tissue in your liver. It can cause the same symptoms as alcoholic hepatitis plus:
- Large amounts of fluid buildup in your belly (the doctor will call it ascites)
- High blood pressure in the liver
- Bleeding in your body
- Confusion and changes in behavior
- Enlarged spleen
- Liver failure, which can be fatal
Alcohol-related fatty liver disease usually comes first. It can then get worse and become alcoholic hepatitis. Over time, it may turn into alcoholic cirrhosis.
If you drink heavily, talk with your doctor. It’s confidential, and they can help you get your drinking under control to save your health.
Symptoms
With ALD and NAFLD, there are usually no symptoms. Some people may have signs such as tiredness or pain in the upper right side of the belly where your liver is.
If you have NASH or get cirrhosis, you may have symptoms such as:
- Swollen belly
- Enlarged blood vessels underneath your skin
- Larger-than-normal breasts in men
- Red palms
- Skin and eyes that appear yellowish, due to a condition called jaundice
Causes and Risk Factors
For ALD, the cause is too much alcohol. You may be even more likely to get it if you drink a lot and
- Are obese
- Are malnourished
- Have chronic viral hepatitis, especially hepatitis C
The reason why some people with NAFLD have simple fatty liver and others get NASH isn’t known. Genes may be a reason. NAFLD or NASH is more likely if:
- You’re overweight or obese
- Your body doesn’t respond to insulin as it should (called insulin resistance) or if you have type 2 diabetes
- You have high levels of triglycerides or “bad” (LDL) cholesterol, or low levels of “good” (HDL) cholesterol
- You have metabolic syndrome. This is a mix of conditions that make you more likely to get type 2 diabetes and heart disease.
You may not know you have it
The scariest part: If you have it, you probably don’t know it.
NAFLD does not produce the telltale symptoms that cardiovascular disease presents. There are no chest pains to tip you off that your organ is in trouble. The good news, though, is that it’s not difficult to diagnose and is reversal is possible.
What can you do today to start a liver-friendly lifestyle?
- Reduce your overall sugar intake, from the common sources like candy to the less common like crackers or salad dressing.
- Increase color.
- Eat more plants that are brightly hued with shades of green, red, orange, and purple.
- Increase your consumption of omega 3 fatty acids from wild fish (we recommend this), chia and flax seeds, and walnuts.
- Drink less.
- Finally, start moving. Get off the couch, and aim for 10,000 steps a day.
All have been associated with a reduced risk of development or NAFLD. In the meantime, if you feel you are at risk, have a discussion with your physician or dietitian and start giving the one organ you think least about a lot more attention.
Kristin Kirkpatrick, MS, R.D., manager of wellness nutrition services at the Cleveland Clinic Wellness Institute in Cleveland, Ohio
Originally posted 2018-11-24 21:59:50.