As a dietitian in private practice, it’s becoming increasingly common for me to tailor diets for clients who’ve been diagnosed with a build-up of fat in their liver.
If your doctor has told you that you have a fatty liver, take action to reverse it. If left untreated, the condition can be more harmful than you think.
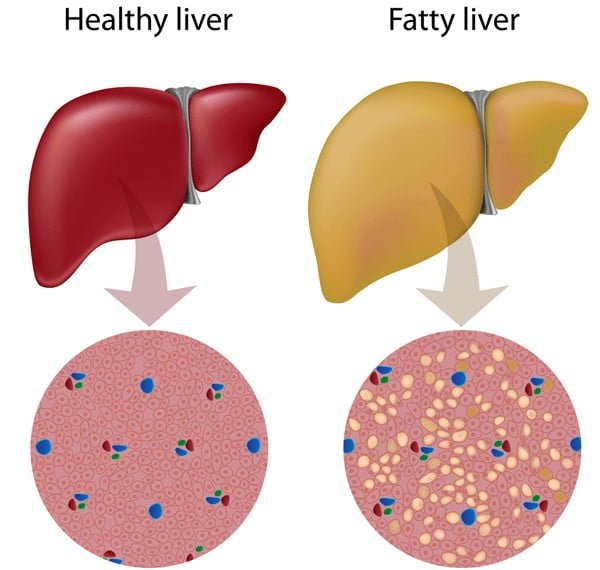
However, a liver infiltrated with fat is more susceptible to further injury.
NAFLD can progress over time to a more severe form called non-alcoholic steatohepatitis (NASH), which is fatty liver accompanied by inflammation and death of liver cells. (Steato means fat and hepatitis means liver inflammation.)
NAFLD also increases the risk of developing heart disease, stroke and Type 2 diabetes.
Prevalence is growing fast
NAFLD is the most common chronic liver disease in Canada and in other western countries. It’s estimated that one in five Canadians has NAFLD, a number that’s escalating in conjunction with the increasing incidence of obesity and Type 2 diabetes. Many people don’t even know they have a fatty liver.
Fatty liver disease isn’t only an adult health problem, it’s showing up in children, too.
According to the Canadian Liver Foundation, one in 10 Canadian children may have NAFLD. And the organization estimates that as many as 53 per cent of obese children have the condition.
The most common cause of NAFLD is obesity. It’s estimated that 75 per cent of obese individuals are at risk of developing simple fatty liver and nearly one-quarter (23 per cent) are at risk for fatty liver with inflammation.
Non-alcoholic fatty liver disease (NAFLD) has numerous causes. Like alcoholic fatty liver disease, non-alcoholic fatty liver disease may be reversed if caught in the early stages. Dietary changes and discontinuing all alcohol will be what it takes to start the fatty liver disease reversal.
Here are some of the causes of non-alcoholic fatty liver disease (NAFLD)
Type 2 Diabetes
Type 2 diabetes is insulin resistance. When someone has insulin resistance, then it’s easy to develop obesity. The obesity and insulin resistance together and by themselves will cause fatty liver disease.
Obesity
The more fat you have in your body, the greater the accumulation of fat in your liver. This then causes fatty liver disease. Losing the weight helps eliminate the fatty liver.
Metabolic Syndrome
Insulin resistance is connected to fatty liver disease because of the high levels of blood fats. Many people with metabolic syndrome eat far too many carbohydrates, which raises triglycerides and ca
As you can see, having diabetes, high blood cholesterol and high triglycerides (blood fats) also increases the likelihood of developing fatty liver disease. Some people, though, don’t have a clear predisposing cause.
The underlying mechanism for fat build-up in the liver is believed to be insulin resistance, often a consequence of obesity and excess belly fat. Insulin resistance means the body’s cells are unable to use insulin properly. As a result, the body needs higher levels of insulin to clear sugar (glucose) from the bloodstream.
Do certain foods cause NAFLD?
A diet that’s too high in fat contributes to excess fat stored in the liver. So does one that’s high in refined carbohydrates and sugars. Liver cells convert excess glucose – the sugar that’s absorbed into the bloodstream after digestion – into fat.
Fructose, in particular, is tied to fatty liver. Studies suggest that fructose consumption not only increases fat production in the liver, it also creates a metabolic environment that favours the development of NAFLD and NASH.
A study published last month in the Journal of Hepatology found that, among 271 children and teenagers with fatty liver disease, fructose consumption was significantly higher in children who had NASH compared with simple fatty liver.

Fructose is a simple sugar found naturally in fruits, some vegetables, honey, agave syrup and sucrose (table sugar). As high-fructose corn syrup (“glucose-fructose” on ingredient lists), it’s also present in many soft drinks, sweetened fruit drinks, breakfast cereals, baked goods and condiments.
Causes of Alcohol-Related Fatty Liver Disease (ALD)
The only cause of alcohol-related fatty liver disease is alcohol. This is obvious to medical experts because those who drink more than two to three drinks daily for long periods of time will often have fatty liver disease – and the fatty liver disease may disappear when the person gives up alcohol.
There are usually no symptoms with alcoholic fatty liver disease. However, some people do experience fatigue, pain in the liver area of the abdomen, and weakness. The cells of the liver are storing large amounts of fat in the form of triglycerides.
Alcohol-related fatty liver disease is not the only liver problem caused by alcohol. Hepatitis can also result. Hepatitis means that the liver cells become inflamed. In fact, in hepatitis, you’ll find the same fat deposition in the liver cells along with inflammation and scarring of the liver. The symptoms worsen with hepatitis and there may be nausea and vomiting, fever and the patient may lose his appetite. His or her skin may also turn yellow because of jaundice.
Alcoholic hepatitis can progress to a severe health condition that results in a quick death. However, it can also be a condition that is reversed. Diet plays a big part in how well the person recovers.

Alcoholic cirrhosis is one additional health problem that is brought on by drinking alcohol. Cirrhosis is the worst because of the scarring in the liver. With scarring, regular liver tissue is replaced with hard, fibrotic tissue that has lost its function. Unfortunately, it’s more difficult to reverse scarring.
When liver conditions progress to the cirrhosis state, there’s edema – swelling – in the abdomen as well as the veins in the abdomen enlarging, called caput medusa because the veins are visible underneath the skin and look like a twisted body of a snake. The condition can progress to kidney failure, coma and death.
If an alcholic shows fatty liver disease, it can then progress to hepatitis and then cirrhosis. It’s not true that fatty liver disease will always progress in this fashion, and sometimes patients who drink a lot of alcohol have hepatitis but not the cirrhosis. One thing is certain though: continuing to drink alcohol will worsen the condition.
So who is most likely to become an alcoholic drinker?
Psychological studies show that those who are dependent on alcohol are people who can’t say no to an extra drink, or the first drink at all. Here’s a list of people who are most likely to become dependent on it:
- Young adults between the ages of 18 and 29 The statistic of those in this age range who binge drink – a habit that can easily lead to fatty liver disease – is as high as 41%.
- Those who tend to be impulsive: Someone who is impulsive will tend to try something on a whim. If friends are encouraging a person to drink all day at a get-together, someone who is impulsive might be more apt to do exactly that. He or she may be in a home situation where feelings of helplessness, hopelessness, frustration and being trapped have been coming up recently, making an impulsive person even more impulsive.
- Those who are influenced by a peer group: Those who are influenced by friends are less apt to stand up for what they believe when the peer pressure is applied.
- Those whose parents drank while they observed the behavior: Watching a parent drink and treat family members poorly is nothing that a child wants to watch. A child can make a decision to never be like the offending parent but then later in life, finds himself or herself walking in the parent’s footsteps. Counseling helps a lot in these cases.
- Those who have had a previous history of drug abuse, and are going through a rough time in their life: Stress brings out the worst in us. A previous history of abusing drugs or alcohol can be ‘relived’ when times get hard, making a person turn to alcohol.
- Those who received accolades for drinking large amounts of alcohol: Getting praised by one’s friends and talked about as if “you’re the man” is a good feeling. But when that feeling is associated with alcohol, it starts a neural pathway in the brain that links happiness with alcohol. This link has to be broken if you are going to give up alcohol, something that is essential to reverse fatty liver. Replacing the happiness with a disgusted feeling (such as imagining maggots in the alcoholic drinks) is an old trick that psychologists and hypnotherapists use to break bad habits.
If you recognize that you could be at risk to develop fatty liver disease as a result of your personal drinking habits, the best choice of health practitioner to see is a psychologist.

Drugs That Cause Fatty Liver
Often the use of drugs is unavoidable, but one of the problems with them is that they may cause harmful side effects such as fatty liver. Any medication that causes a person to gain weight is potentially contributing to fatty liver. Thus, the listing of many drugs associated with fatty liver disease includes the following:
- birth control pills -Drugs to prevent pregnancy are so widely used that the side effects are rarely considered.
- antidepressants – There are many types of drugs that treat depression.
- antipsychotic medications – Drugs that treat psychosis can also cause fatty liver disease.
- valproic acid – This is an anti-epilepsy drug.
- diltiazem – This prescription medication is a heart medication that is called a calcium channel blocker.
- indinavir – You wouldn’t know much about this prescription medication unless you had HIV. It’s a drug reserved for those who have HIV.
- tamoxifen – This is a prescription drug based on an ingredient from the Pacific Yew tree. It’s used as an anti-estrogen medication for those who have breast cancer and is part of the treatment plan for cancer patients.
- high dosage of intravenous tetracycline – You have to be pretty sick to end up with a high dosage of intravenous tetracycline. It’s one that is used in the Intensive Care Unit in the hospital.
- alcohol – As little as two drinks a day for women and three drinks a day for men can cause the appearance of fatty liver disease.
- cigarettes – Fatty liver disease is one of those hidden health problems of cigarettes you never thought of.
- sedatives – These are drugs that calm you down.
- corticosteroids – Two primary steroid drugs are cortisone and prednisone.
- methotrexate – This is a potentially-dangerous medication used as a last resort for rheumatoid arthritis.
- Amiodarone – This medication treats abnormal heart rhythms.
- sulfonamides – This medication treats infections; these drugs also use up para-amino-benzoic acid (PABA), a B vitamin, in the body which is used to synthesize folic acid in the intestines.
- phenytoin – This anti-epilepsy medication is especially used for grand mal seizures.
- antithyroid drugs – The primary medication in this category are the ones used for hyperthyroidism.
- phenothiazines – These drugs treat schizophrenia and other psychotic disorders.
- salicylates – These are aspirin-based medications that treat mild to moderate pain.
How These Drugs Harm the Liver
When drugs harm the liver and cause fatty liver, they cause the elevation of liver enzymes. Three of the most important liver enzymes are found on liver function tests, and are called SGOT or AST for short, ALT or SGPT, and alkaline phosphatase.
There are three types of liver injuries:
1. Hepatocellular injury – If this type of injury shows jaundice as one of the symptoms, the person may be a candidate for a liver transplant. Two drugs that can cause this injury are acetaminophen and isoniazid as well as the gout medicine allopurinol; NSAIDS Omeprazole, Paroxetine, Rifampin, Sertraline; Lisinopril, Losartan and Methotrexate, Baclofen, Statins, Tetracyclines, Trazodone, and Risperidone. The injury is reflected in elevated ALT enzymes.
2. Cholestatic – This type of injury is not as bad as hepatocellular injury, but it may destroy the bile ducts and cause itching skin as well as jaundice. Cholestatic injuries show high alkaline phosphatase and total bilirubin. Drugs that cause it include oral contraceptives, amoxicillin, estrogens, Mirtazapine, Terbinafine, Phenothiazines, Erythromycins, and Anabolic steroids.
3. Mixed – This injury is reflected by similar lab test findings as the hepatocellular injury and the cholestatis injury. It’s caused by the drug phenytoin. Drugs responsible include Amitriptyline, Captopril, Sulfonamides, Trazodone, Verapamil, Phenobarbital, Clindamycin, Carbamazepine, and Trimethoprim. Treatment for these liver injuries starts with removal of the prescription medication causing them.
How do you know if you have a fatty liver?
Fatty liver rarely causes symptoms. When it does, symptoms are vague and may include right-sided abdominal pain, fatigue and/or a general feeling of unwellness.
NAFLD is usually detected when routine blood tests show elevated liver enzyme levels. It can also be discovered by an ultrasound examination of the abdomen.
How can you get rid of a fatty liver?
Lifestyle modification is the cornerstone to treating – and preventing – non-alcoholic fatty liver disease. Gradual weight loss, dietary modification and exercise are required to effectively remove fat deposits in the liver.
A diet plan for fatty liver disease
Lose excess weight
Weight loss is the most effective treatment for NAFLD. A 5-per-cent weight loss can reduce liver fat deposits and a 10-per-cent loss is required to improve fatty liver with inflammation (NASH).
Lose weight gradually at a rate of one to two pounds a week. Rapid weight loss (four pounds a week or more) can worsen fatty liver.

Restrict refined grains
Limit your intake of high glycemic foods such as white breads and crackers, refined breakfast cereals and white rice. These foods spike glucose and insulin levels and may contribute to a fatty liver.
Choose fibre-rich whole grains such as brown rice, quinoa, whole wheat pasta, 100-per-cent whole grain breads and cereals and oatmeal, foods that raise blood glucose gradually, not quickly.
As a source of prebiotics (fibrous carbohydrates), whole grains also help feed beneficial gut bacteria. Some evidence suggests that an altered gut microbiome plays a role in fatty liver disease.
Don’t overdo carbohydrates, though. A lower carbohydrate diet is beneficial for fatty liver disease.
Reduce sugars
Keep your intake of added sugars to no more than 5 per cent of daily calories, about 24 grams (6 teaspoons worth) for women and 36 grams (9 teaspoons worth) for men.
Avoid sugar-sweetened beverages, whether they’re made with high-fructose corn syrup (fructose-glucose) or not.
Limit use of all caloric sweeteners including honey and agave syrup that are high in fructose. Read labels and, as much as possible, avoid foods sweetened with glucose-fructose.
Choose healthy fats
A diet that’s lower in total fat and saturated (animal) fat will help improve fatty liver. Diets high in saturated fat have also been shown to induce insulin resistance.
Emphasize monounsaturated fat, the type found in olive oil, peanut oil, canola oil, avocado, almonds, cashews and pecans. Monounsaturated fat has been shown to increase fat breakdown and it may have anti-inflammatory benefits.
Eat fatty fish (e.g., salmon, trout, sardines) twice a week to get anti-inflammatory omega-3 fatty acids. If you have high blood triglycerides, speak to your dietitian or doctor about fish oil supplementation.
Boost antioxidant foods
Free radical damage, or oxidative stress, plays a key role in liver cell damage. Eat foods rich in dietary antioxidants such as citrus fruit, berries, mango, leafy green vegetables, carrots, sweet potato and nuts and seeds.
Avoid alcohol
If you have NAFLD or NASH, avoid drinking alcohol as it puts extra stress on your liver.
Increase exercise
Include at least 30 minutes of aerobic exercise five times a week and resistance training twice weekly. Doing so can improve fatty liver, lower blood sugar and reduce the risk of heart disease regardless of weight loss.





0 thoughts on “Fatty Liver Diseases: Causes and diet plans”